Recently, I had the opportunity to see a young boy in my clinic, a great little guy who had had a bit of a rocky start to life. He had been born four months premature, and had sustained an intraventricular hemorrhage, a type of bleeding within the brain that is, unfortunately, quite common in severely premature infants. To reduce the swelling and pressure in his head created by this bleeding, a shunt was placed, which drained fluid from around the brain into his abdomen.
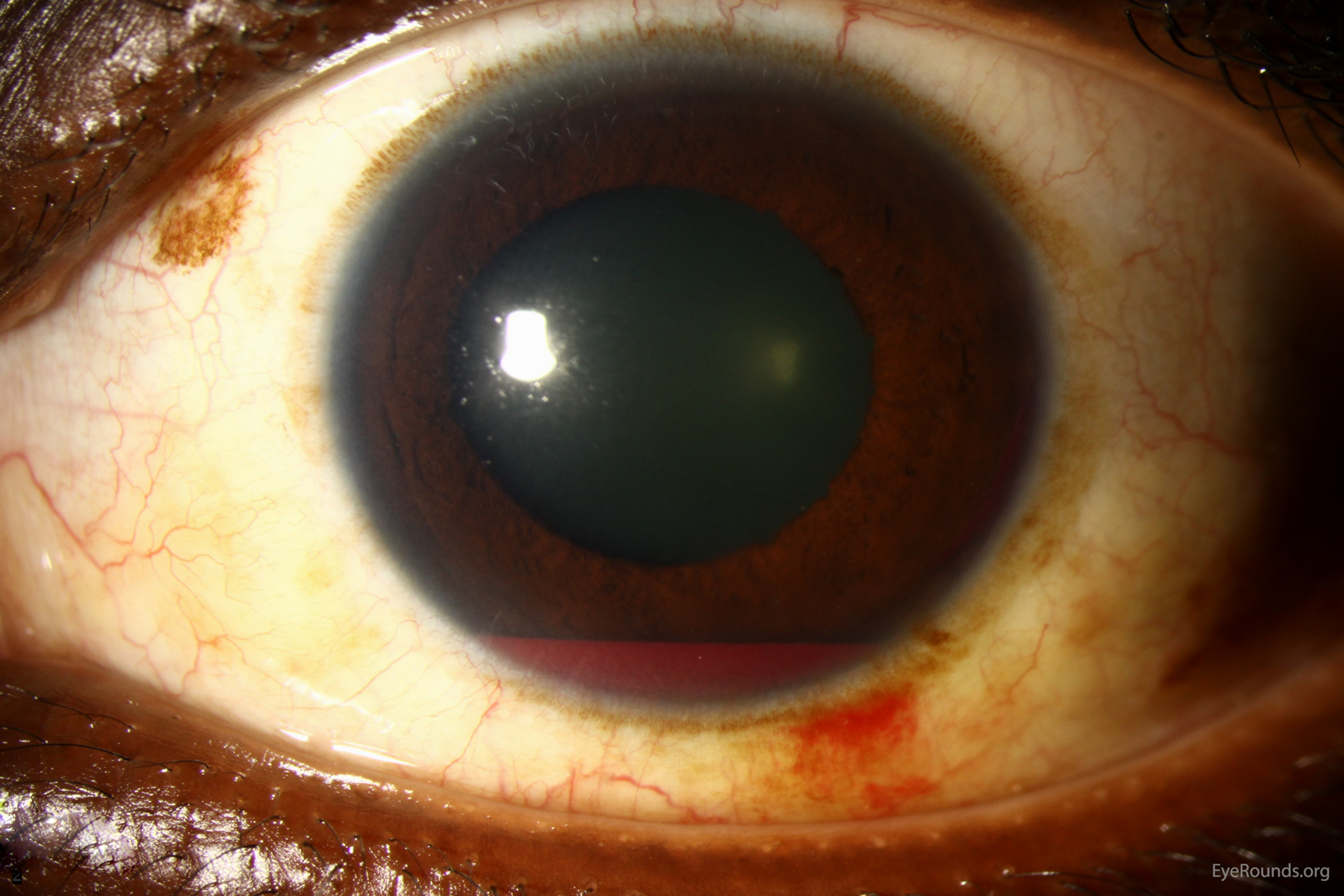
Between this brain hemorrhage and a number of other medical problems, my little patient's first few years were tough. His mother had been told that, because of the swelling, he had likely suffered some damage to his optic nerves, the structures that connect the back of the eye to the brain, and transmit the signal that the eye sees to the cerebral cortex for processing.
Fortunately, when I examined his eyes, I was able to get a good look at his optic nerves, and they appeared very healthy -- flat and pink, just like they should be, with no swelling, pallor, or hemorrhage. I told Mom that her son's optic nerves looked great, and that I was encouraged by that. Her response caught me off guard.
She said, somberly but matter-of-factly, "That's great. We never get good news."
This made me feel very sad.
One of the blessings of my job is that I work with kids all day -- kids who are often, though not always, generally quite healthy. This means that my experience in the "doctor's office" (in this case, my own), is usually very positive and full of good news.
This young family, by contrast -- and many others like them -- has a much different typical doctor's office experience. Because of the many, severe health problems their son has dealt with, his physicians have, unfortunately but appropriately, had to give an awful lot of bad news.
Sometimes as physicians, we may forget how devastating a seemingly endless parade of bad news can be.
My friend Dr. Erin Schotthoefer, a fellow pediatric ophthalmologist who also did her ophthalmology residency at the University of Iowa like I did, taught me something very profound. During a lecture given 10 years after finishing her training, she told the audience that, for every patient she saw, she always tried to find at least one bit of good news she could share, one thing about which the child's parents should be happy and encouraged.
Inspired by her words, I have tried to do the same in my practice, and have found it both possible and powerful. Sometimes, we all just need something to hold on to, and findings those things and sharing them is one of my favorite parts of what I do.