While wandering through the greenhouse at beautiful Manito Park here in Spokane recently, I came across this plant:
I had never seen a Dieffenbachia before, and I must admit I recoiled a bit. The reason? The sap of this plant contains needle-like crystals, which, if they contact the eye, can lodge in the cornea, the clear layer in front of the iris, or colored part of your eye. Although these crystals dissolve spontaneously over several weeks to months, while present, they cause intense eye pain and sensitivity to light.
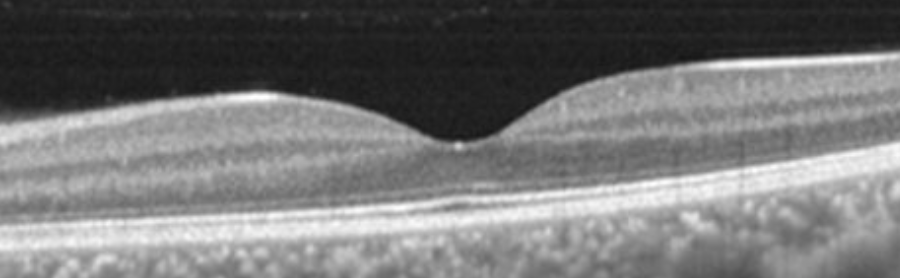
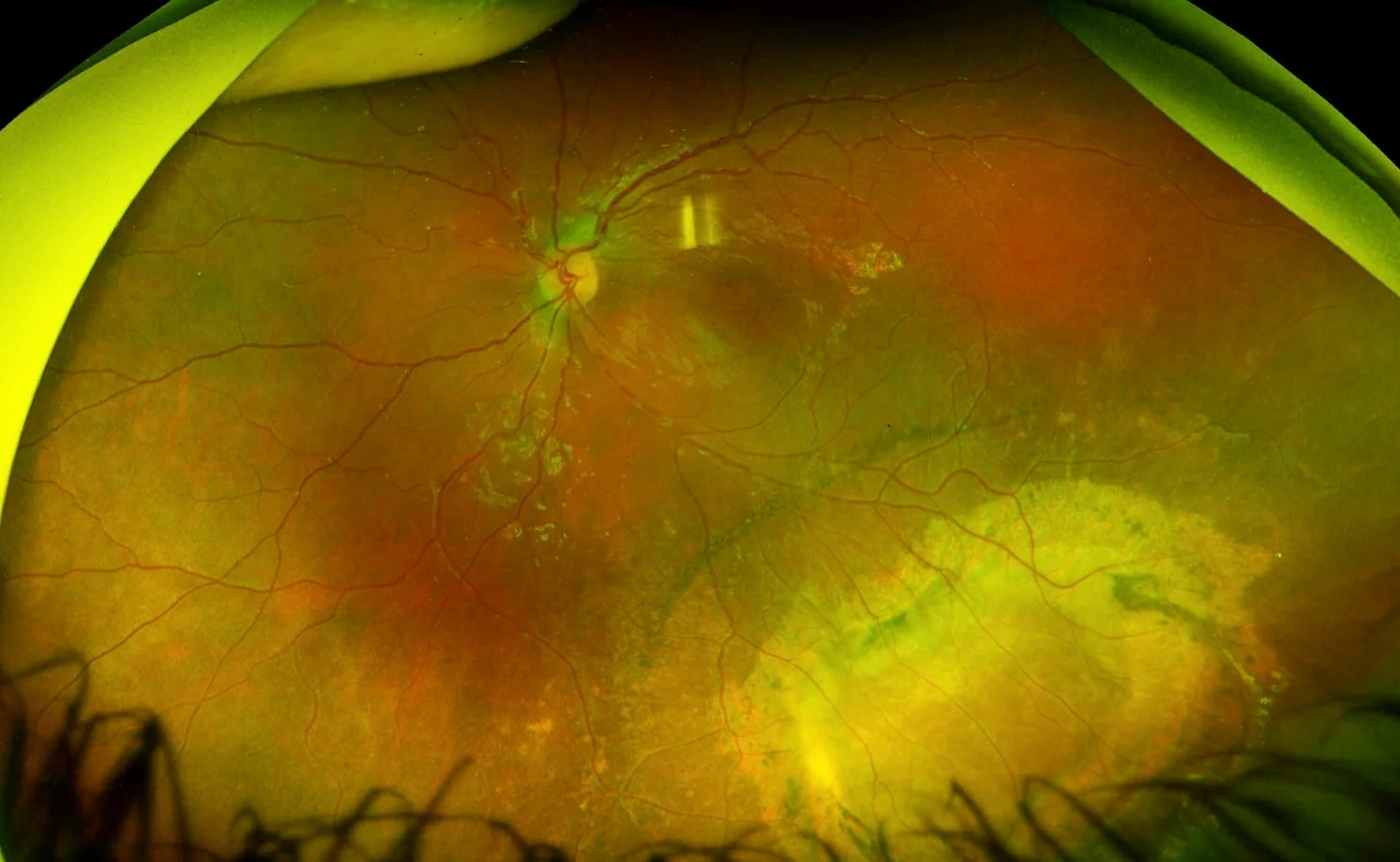
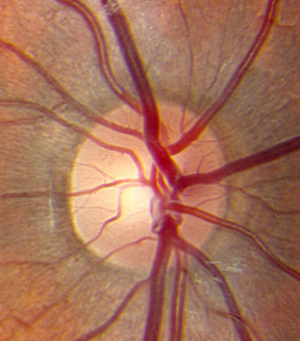
The cornea is the clear layer at the front of the eye, through which light passes. If it is disrupted, pain and light sensitivity often result.
These crystals, made up of calcium oxalate, are found in tiny structures in the leaves and stem of the plant known as idioblasts. These idioblast cells, when stimulated by even mild pressure, rupture, and forcefully expel their contents onto unsuspecting onlookers.
Interestingly, the plant is named after the German physician and botanist Joseph Dieffenbach. Its first name, however, was "dumbcane," because the painful swelling of the tongue caused by chewing it would render a person effectively unable to speak. Also of note, Dr. Dieffenbach is particularly near and dear to my heart as a strabismus surgeon, because he was the very first surgeon to weaken the medial rectus muscle to treat esotropia.
Be sure to give these plants wide berth next time you see them!